Fluorescent sensors provide a distinctive look into live cells since they may be used to identify and picture a broad range of substances. However, because their signal is lost when they are implanted too deeply, they are often only effective in cells grown in a lab dish or in tissues near to the surface of the body.
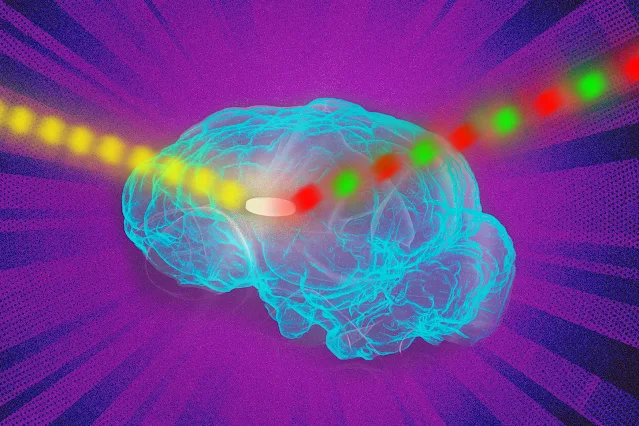
Now, MIT engineers have found a means to get around that restriction. They were able to significantly enhance the fluorescent signal by using an unique photonic method they created for activating any fluorescent sensor. The researchers demonstrated that with this method, sensors may be implanted up to 5.5 centimeters deep in tissue and still get a good signal.
According to Volodymyr Koman, a research scientist at MIT and one of the study's lead authors, "this technology allows you to translate all of those fluorescent dyes and probes into thick tissue if you have a fluorescent sensor that can probe biochemical information in cell culture, or in thin tissue layers."
The principal author of the work, which was published in Nature Nanotechnology today, is Naveed Bakh, SM '15, Ph.D. '20. The study's principal author is Michael Strano, the Carbon P. Dubbs Professor of Chemical Engineering at MIT.
An increase in fluorescence
Quantum dots, carbon nanotubes, and fluorescent proteins are just a few of the various fluorescence sensors that scientists employ to mark molecules inside cells. By placing laser light on these sensors, the fluorescence may be seen. However, because tissue itself also produces some fluorescent light, this does not operate in tissue that is thick, dense, or deep within tissue. The signal from the sensor is overpowered by this light, known as autofluorescence.
All tissues undergo autofluorescence, which turns out to be a limiting factor, claims Koman. The tissue autofluorescence overtakes the sensor's signal as it gets weaker and dimmer, according to the study.
The MIT team devised a method to modify the frequency of the fluorescent light generated by the sensor in order to get around this restriction and make it easier to distinguish it from tissue autofluorescence. Three lasers are used in their process, which they refer to as wavelength-induced frequency filtering (WIFF), to produce a laser beam with an oscillating wavelength.
The frequency of the fluorescence that the sensor emits doubles when this oscillating beam shines on it. This makes it simple to distinguish the fluorescent signal from the autofluorescence in the background. The signal-to-noise ratio of the sensors was improved more than 50 times by the researchers' use of this technology.
Monitoring the efficiency of chemotherapy medications is one potential use for this type of sensing. The researchers concentrated on glioblastoma, an aggressive form of brain cancer, to show this potential. Patients with this kind of cancer often have surgery to remove the tumor in its entirety, followed by temozolomide (TMZ) chemotherapy to try to eradicate any cancer cells that may still be present.
According to Strano, it would be beneficial to have a simple way to track whether or not this medication is functioning because it can have major adverse effects and it doesn't work for all people.
You could implant a sensor near the tumor and assess from the outside the efficacy of the drug in the actual tumor environment, he says. "We are working on technology to make small sensors that could be implanted near the tumor itself, which can give an indication of how much drug is arriving at the tumor and whether it's being metabolized."
Temozolomide is broken down into smaller compounds when it enters the body, one of which is AIC. The MIT researchers created an AIC-detection sensor and demonstrated that they could implant it as deep as 5.5 cm into an animal's brain. Even through the animal's skull, they were able to interpret the sensor's signal.
The development of such sensors may potentially enable the detection of molecular markers for tumor cell death, such as reactive oxygen species.
Whatever wavelength
The researchers showed that WIFF may be used to boost the signal from a range of different sensors, such as carbon-nanotube-based sensors that Strano's group has previously created to detect hydrogen peroxide, riboflavin, and ascorbic acid. In addition to detecting TMZ activity.
According to Strano, the method may be applied to any fluorescence sensor and is effective at any wavelength. You can implant a sensor into tissue at depths that were previously impossible since there is so much more signal available now.
In order to produce the oscillating laser beam for this study, the researchers used three lasers; but, in further work, they intend to employ a tunable laser to create the signal and advance the approach even further.
According to the researchers, this should become more practical as tunable lasers get cheaper and quicker.
The researchers are developing physiologically resorbable fluorescent sensors so they wouldn't require surgical removal in order to make fluorescent sensors more convenient to utilize in human patients.